Facing a breast cancer diagnosis turns a woman’s life upside down. Once the treatments are over, many new moms ask themselves an important question: “Can I breastfeed after breast cancer?”
That question carries a mix of emotions, medical concerns, and a deep desire to give the best to their baby.
This article explains what’s possible, what the limits are, and what support you can find across Canada to guide you through this sensitive stage.
Can You Breastfeed After Breast Cancer?
There isn’t one simple answer; it depends on many factors. The type of treatment you received, the length of your remission, and the condition of your breast tissue all matter.
If you had breast-conserving surgery, you may be able to breastfeed with the breast that wasn’t treated, or sometimes even partially with the treated one.
If radiation therapy affected the breast tissue, milk production often becomes permanently reduced or stops entirely.
After chemotherapy, you need to wait until all medication has left your body, since these drugs pass into breast milk and can harm your baby.
In short, every case is different. That’s why you should always talk to your oncologist and, ideally, a lactation consultant before making a decision.
How Treatment Affects Breastfeeding
Every type of breast cancer treatment impacts breastfeeding differently.
Breast Surgery
After a full mastectomy, breastfeeding with the affected breast isn’t possible. If only one breast was removed, the other can still produce milk, though sometimes not enough for feeding exclusively through this method.
Radiation Therapy
Radiation permanently damages breast tissue. The treated breast usually can’t produce milk or produces very little. If the other breast wasn’t treated, it can still supply milk for partial or full feeding.
Chemotherapy and Hormone Therapy
Breastfeeding during chemotherapy is not safe because the drugs will be present in the breast milk. After treatment ends, you need to wait long enough for all medication to clear out of your system.
Hormone therapy, which often lasts for years, also makes breastfeeding impossible.
When Breastfeeding Becomes Possible Again
You may be able to breastfeed after breast cancer if:
- You’ve finished all active treatments, and your doctors confirm no toxic substances remain in your system.
- You have one breast unaffected by surgery or radiation that can still produce milk.
- Your overall health allows it, and your doctors confirm that breastfeeding won’t compromise your recovery.

In some cases, partial breastfeeding is possible; you can nurse while supplementing with formula. Even partial breastfeeding is a valuable emotional, nutritional and bonding experience for you and your baby.
The Emotional Benefits of Breastfeeding After Cancer
For many survivors, breastfeeding feels like more than just feeding a baby; it’s a personal victory and a symbol of renewal.
It’s a way to reclaim your body after months or years of illness and treatment.
It’s a way to experience motherhood on your own terms, despite your medical history.
And it’s an intimate, comforting moment that helps emotional healing.
Every drop of milk becomes a gesture of courage and love, a sign that life goes on.
If Breastfeeding Isn’t Possible
If you can’t breastfeed, you still have safe, nurturing options for your baby:
- Pumping: Even a small milk supply can be collected and offered to your baby.
- Milk banks: In several regions of Canada, it’s possible to obtain pasteurized donor milk, especially for premature babies.
- Infant formula: Safe and reliable, it can be used alone or combined with breast milk.
What truly matters is your well-being and your baby’s. The love, closeness, and care you give go far beyond your feeding method.
Support and Resources in Canada
Many organizations in Canada support women who want to breastfeed after breast cancer:
- The Canadian Cancer Society offers phone support and reliable information.
- The Canadian Partnership Against Cancer helps improve access to care and resources.
- Specialized lactation clinics often collaborate with oncology departments to provide personalized guidance.
Surround yourself with professionals and peer support. Talking with other mothers who’ve lived similar experiences can be incredibly healing.
Practical Tips for Moms After Breast Cancer
If you’re considering breastfeeding after cancer, keep these tips in mind:
- Talk to your doctors: They know your medical history best and can confirm what’s safe.
- Prepare early: Learn how your treatments may have affected milk production.
- Accept your body’s reality: Partial breastfeeding is still a success.
- Seek support: A lactation consultant can guide you step-by-step.
Be kind to yourself: You’ve already been through so much; don’t add pressure.
FAQ: Breastfeeding After Breast Cancer
Yes, you can. The untreated breast may produce enough milk, though sometimes supplementation is needed.
It depends on the drugs used. Only your oncologist can confirm when it’s safe to start.
No, studies show that breastfeeding doesn’t raise recurrence risks. It actually supports your overall health.
You can turn to the Canadian Cancer Society, the Canadian Partnership Against Cancer, and local lactation clinics for guidance and support.
Breast Cancer Awareness Day: Supporting Mothers and Raising Awareness
Every year on October 19, Breast Cancer Awareness Day highlights the importance of prevention, screening, and support for women affected by breast cancer.
It’s also a chance to open up conversations about motherhood after cancer.
If you’re a new mom or planning to become one after a diagnosis, you’re not alone. Organizations such as the Canadian Cancer Society and the Canadian Partnership Against Cancer offer programs and resources designed for you.
Breast Cancer Awareness Month reminds us that every story is unique and every mother deserves compassion and support.
Breastfeeding and Cancer: Key Takeaways
Breastfeeding after remission is sometimes possible, but not always. Each journey is unique, and only your medical team can tell you what’s safe.
If breastfeeding isn’t possible, it doesn’t define your motherhood. What matters most is your connection with your baby, and your health.
We encourage you to learn everything you can, ask questions, and find the right support system. After cancer, every moment of life matters, and every choice deserves respect.
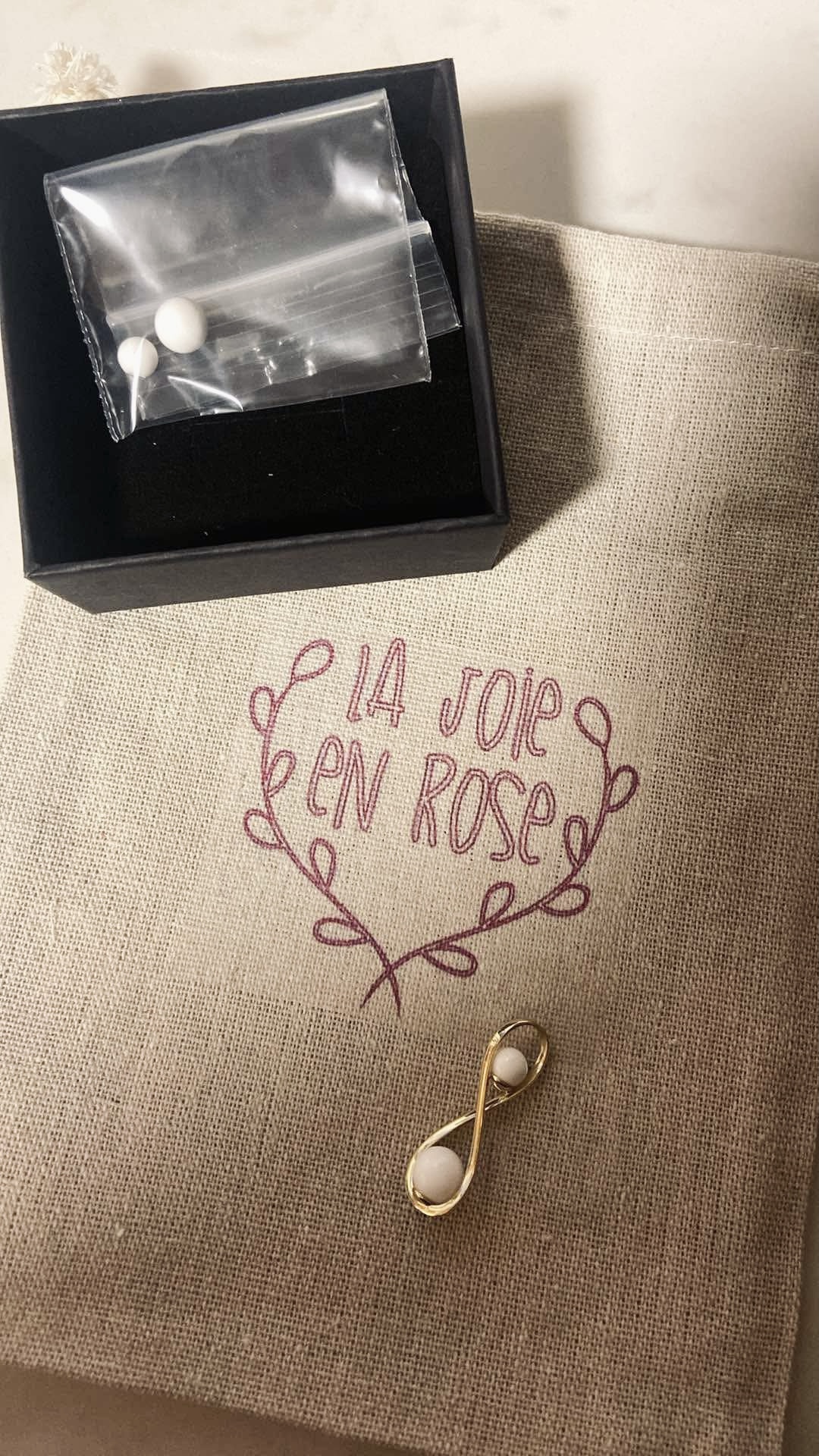
La Joie en Rose proudly supports the Canadian Cancer Society.
For each Seins jewellery piece sold, $10 is donated to the Canadian Cancer Society.
«One in eight Canadian women will face a breast cancer diagnosis in her lifetime, and more than 25,000 receive this diagnosis each year.
Help make a difference in women’s lives and for future generations by supporting the Canadian Cancer Society’s mission.»


Comments are closed for this article!